The Sainsbury Centre For Mental Health Patient Choice Tangle Angles
What has been clearly established in the preceding stories (Here 1 and Here 2) is there is no UK legal equivalence of Patient Choice in Mental Health. You cannot choose a secondary care provider and or have a choice of consultant on the first appointment even if you are not "sectionable" under the 1983 Mental Health Act ....
We have shown the key Jan 2009 document that erases all Patient Choice in UK Mental Health.
Where was the loud protests from the Mental Health Charities ? Well there were some statements here and there but little real action to safeguard equal rights of Patient Choice in Mental Health .
Mostly the mental health charities energies went into the strands of compromise with a system that feeds their careers all too often as they became both closer and closer advisors over the years 2000 - 2010 to Gov't and finally recipients of big lottery and other grants that were given for policies they had actually shaped . Who is better off then ?
Careerists inside the charities ? Quango agencies all pushing the mental health User-herds into work corrals that do not in fact exist ? What were the lost opportunities this form of development took away ?
Was it individualised Patient Choice of recovery ? A new mental health recovery culture that developed and grew . Yes it was partly .
Patient Choice of talking therapies might have been the first gateway possible with the GP axis and some purchasing power being used intelligently at that point and both State and private supply sides of therapy being a competitive choice and quality driver. Labour took the GP purchasing mechanism away though which existed in the late 1990's . It feared the GP's as drivers and market ideas , and so did others, but "Patient Choice" was a concept driver that was created by Labour as a prioritising ability that over-ruled GP's . Why fear that ? GP Practice Based Commissioning bodies (read on) could have created local talking therapy choices in mental health and piloted those . Certainly GP's in their recent March 22nd 2010 survey demonstrated a nationwide impoverished lack of talking therapy services in 2010 with 65% claiming therapy access for adults was rare and the figure for children was 78% claiming access was rare .
Labour prior to 2004 put forward the Practice Based Commissioning ( pro-choice) method in which GP's could cluster on a local basis and bid for Primary Care Trust funds to target local population health needs where they indicated a good argument for better service supply . The PBC's have been very slow to develop under Labour despite the need for local sensitivity in targeting unmet health need.
Sainsbury Centre For Mental Health had this to say about PBC's and mental health in 2004 :
We have shown the key Jan 2009 document that erases all Patient Choice in UK Mental Health.
Where was the loud protests from the Mental Health Charities ? Well there were some statements here and there but little real action to safeguard equal rights of Patient Choice in Mental Health .
Mostly the mental health charities energies went into the strands of compromise with a system that feeds their careers all too often as they became both closer and closer advisors over the years 2000 - 2010 to Gov't and finally recipients of big lottery and other grants that were given for policies they had actually shaped . Who is better off then ?
Careerists inside the charities ? Quango agencies all pushing the mental health User-herds into work corrals that do not in fact exist ? What were the lost opportunities this form of development took away ?
Was it individualised Patient Choice of recovery ? A new mental health recovery culture that developed and grew . Yes it was partly .
Patient Choice of talking therapies might have been the first gateway possible with the GP axis and some purchasing power being used intelligently at that point and both State and private supply sides of therapy being a competitive choice and quality driver. Labour took the GP purchasing mechanism away though which existed in the late 1990's . It feared the GP's as drivers and market ideas , and so did others, but "Patient Choice" was a concept driver that was created by Labour as a prioritising ability that over-ruled GP's . Why fear that ? GP Practice Based Commissioning bodies (read on) could have created local talking therapy choices in mental health and piloted those . Certainly GP's in their recent March 22nd 2010 survey demonstrated a nationwide impoverished lack of talking therapy services in 2010 with 65% claiming therapy access for adults was rare and the figure for children was 78% claiming access was rare .
Labour prior to 2004 put forward the Practice Based Commissioning ( pro-choice) method in which GP's could cluster on a local basis and bid for Primary Care Trust funds to target local population health needs where they indicated a good argument for better service supply . The PBC's have been very slow to develop under Labour despite the need for local sensitivity in targeting unmet health need.
Sainsbury Centre For Mental Health had this to say about PBC's and mental health in 2004 :
"The Government recently set out new plans for general practitioners (GPs) to commission a range of specialist health services for their patients. The plans, called practice based commissioning, allow for budgets to be devolved from primary care trusts (PCTs) to individual practices.
The scope of practice based commissioning includes most mental health services. The Sainsbury Centre for Mental Heath (SCMH) is concerned that this may be premature. There is a risk that the payments system for mental health care (which will soon be different to many other NHS services) will put cost above quality and patient choice in making decisions about what to commission.
While there are important benefits to the new system, SCMH recommends that practice based commissioning is not extended to mental health services until it can be done on an equal basis with other parts of the NHS. "
It seems this kind of SCMH advisory tack was also taken forward and consolidated in 2005 as Richard Layard gave his September 2005 speech at the SCMH centre about promoting Cognitive Behaviour Therapy and access to it. He advised access was not to be being governed by the GP route but by a new trained workforce . Its at that point that once again Patient Choice is defeated and the State takes over with its now often criticised one-size CBT fit as opposed to using a mixed economy approach which creates Patient Choice possibility . GP's could have been aided by PCT's to ensure a provisioned approach which created a market and patient quality questionnaire/outcome measuring . There were operable ways to do that .
Richard Layard stated of his own ideas on State governed training (which seperated itself off from all other psychotherapy supply in the market community) that CBT was "evidence based" and that various critiera had to be met ideally to deliver it . (SEE FULL SPEECH)
"These criteria cannot be satisfied within a system of GP-led provision, and I suggest that the new offer of therapy to people with depression and anxiety disorders be delivered through treatment centres.
Why?
· They would provide a much better framework for the supervision of casework and for in-service training and professional development than would a service run by GPs.
· They would make it possible to monitor whether therapists were achieving results through standard self-assessment measures where results were made available to the senior staff of the Centre.
· They would make it easier to organise the right therapist for each patient, and reduce the chanciness of whether your own GP practise has the therapist you need. They would make it easier to organise the effective use of human and physical resources, due to economies of scale.
· They could provide a route of self-referral for patients who did not want their GPs to know about their problem."
But what became the State IAPT roll out (Improvment In Accessing Psychological Therapies) used up a lot of money immediately to train up graduates for CBT and the question was why capacity for patient outcome measuring was not built into PCT community worker managment and private therapy supply used ? Well of course we all know that State central control was favoured at all times and argued as more efficient . But was it more efficient ?
In 2005 Jenny Rankin of IPPR (Institute for Public Policy Research) wrote a paper on Mental Health Patient Choice (working Paper 3) supported by Rethink . What was partly refreshing about her approach was the part-demystification of what Patient Choice in mental health meant . Where it might really go .. Into a new landscape. Has it got there though ?
"Choice means the power to make decisions. It goes beyond ‘voice’ mechanisms, such as surveys and consultations. It is more specific than ‘personalisation’ and the amorphous concept of ‘modernisation’, although it is undoubtedly part of both these agendas.
In their manifesto for the General Election of 2001 the Labour Party promised to give patients more choice in the health service (Labour Party 2001). Although at that time, choice was more aspiration than policy, it has since been spelled out as meaning choice of provider in elective surgery, as well as greater convenience for patients.
In mental health, the choice agenda has had a different evolution to the development of choice in the rest of the NHS. Arguably, it has been shaped by mental health’s unique history.
People with mental health problems have been stigmatised, subject to poor practice or not taken seriously (Prior 2003). The underlying assumption of past mental health services was that patients were unable to make choices. Also unique to mental health are the coercive aspects of the service. As such, choice poses a significant challenge to established ways of delivering services and interacting with people. In the long run, the concept of choice could have a transformative effect, both on how mental health services work, as well as how society responds to mental health problems. These are the themes this paper will explore."
Jenny Rankin writes further on in the paper :
"Following these principles, this paper makes two recommendations. First, the GP should no longer be the sole gatekeeper into services; instead there should be new ways to access mental health support through different types of worker based in community organisations.
Secondly, people should be entrusted with their own personal recovery budgets, adapted from the current practice of direct payments. This would require pilots to test how joint health and social care personal budgets work in practice. In turn choice will only become a reality, if certain conditions are put in place. In particular, this paper singled out extended resource capacity, better commissioning, use of individual care plans, a change in professional attitudes, creating roles for professionals and independent advocates to support choice and good information. Resources are a key issue here; the current allocation of resources does not reflect people’s preferences, and there are high levels of unmet demand for certain treatments, especially talking therapies. "
Where that paper's directions failed we think was in two ways . The GP axis of importance was underestimated almost as if GP's were part of the problem rather than the solution and also "market supply" is not openly spoken enough of as more options for Patient Choice . Its as if the CBT supply (in the talking therapies which came on stream patchily in 2010 ) and new workers in community organisations were going to take the place of real Patient Choice options which should have included partly the market. Yet therapy supply from the market was shut down on the back of arguments with private therapists pressured to come under State regulations despite having their own code of ethics , complaints processes and being able to be selected as approved providers or not by PCT's . Some PCT's as a matter of approving supply had in fact approved counsellors previously . The experience was there. It was not built on though .
It seems the paper has to be partly decoded inside the political and social context it was made and within the mental health Charity orbit of interests.
There are good Patient Choice points (Page 19) about vouchers for therapy that Jenny Rankin mentions but they have never crystallised very fully and appear to be rolled out very minimally :
"Personal recovery budgets
The NHS has often proved fairly unresponsive to people’s demands for different kinds of services, notably talking treatments. Introducing greater individual budget holding, through direct payments or specific vouchers for talking therapies could help to remedy this. If people were given their own personal recovery budget they could choose their own treatment. This would also help correct a theoretical anomaly where people (at least, those who are eligible for community care) have choice in social care, but not in health care."
Did we get Patient Choice in Mental Health UK legally recognised ? No . Not at all . Did people get talking therapies yet ?
Jenny Rankin also re-stated John Reid's much quoted Secretary Of State July 2003 statement : from Page 9 :
“Trust me, I’m a patient” should be the guiding principle of [the] new agenda.
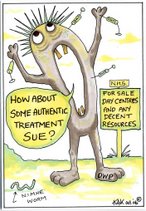
We are still waiting to be trusted and in fact are often as patients inside a new inequality-form of partly invisibilised existential strait jacket designed by the State for the State's application on us and provoking people sometimes into being "in a state" .....We still have a State recipe for continuing illness. There's no choice .
further refs
Choice 2007 docs


.jpg)




No comments:
Post a Comment