What The Service Users Said : Question 12 :
"if there are problems in your personal treatment /support experiences of the services locally to you can you state what they are concisely "
1..... Rude psychiatrist. No real explanation and shit cover apart from by my own CPN.
2..... They are inconsistent and poor at seeing my needs as well as giving me the help I feel I need - I just want therapy and to be heard empathetically and to manage my damage and to create a life that I can live with some real emotional help .
3..... Complete lack of options regarding recovery models. Lack of response, support, and on delivery of promises in several instances.
4......No personal service
5...... I am not offered any support with my local CMHT and having to look at out of area CMHT for much needed support
6....... I've only ever been offered a CPN to deal with present issues rather than some long term therapy to learn to deal with and understand the more deeper issues.
7.......Psychiatrists reluctance to prescribe meds. They should listen to what we need, as we know best.
8......Now have a social worker that I cannot relate to and don't trust to talk to.
9.....Have only been diagnosed with BP.D. 8 months but been diagnosed with lot of other things in the past and I have felt that since BP.D. diagnosis attitude of Psychiatrist Doctor etc.. has changed negatively toward me
10.....Just having to get appointment it is a long wait I have been waiting 9 months
11.....I currently have an in depth treatment plan, I see a CPN for counselling and support fortnightly, a psychologist for CAT weekly and a psychiatrist for review 3 monthly. It has taken a lot of struggling over an 8 year period and many hospitalisations to get this. However all of this is due to end in September a mere 6 months after it commenced. It has been indicated that at that time I shall be discharged from all services regardless of my MH state. Lack of communication, I have to inform my psychiatrist of when I've been to hospital.
12.... Often it has felt like there is little available in terms of prevention and everything is focused on picking up the pieces afterwards. I now see a psych liaison nurse occasionally but for her to see me is essentially above and beyond the call of duty. I suspect that past crises could have been avoided if I had received support I needed to sort myself out before things got too much to handle.
13...What services?
14.....The only treatment they offer me now apart from drugs is group therapy which I'm not sure is right for me but they say there is no more individual treatment available for me
15.....No support from secondary services is allowed because I am encouraged to manage on my own, regardless of how bad I feel. I was turned down for a social worker when I hadn't opened mail for a year and was about to be evicted, which resulted in a suicide attempt and a month in hospital.
16......Inconsistency & changes
17.....Major failure in several aspects....Sending letters to wrong addresses, not taking my condition seriously :(
18....A lack of communication and understanding of the disorder or a lack of willingness to want to understand!!! Lack of crisis intervention and respite care short term.
19.....Not being taken seriously, being discharged when in severe need of help.
20.....Despite direct referral from England CPN to Mental Health services here (6yrs ago), have only just got a CPN in last 6 months (different system, & fell between 6-wk/short-term CPN & not fitting 'tick boxes' for longer-term). Have had consultant, but deteriorated without support. Long wait (told 1-2yrs) for DBT/CAT, but haven't been referred for any therapy anyway yet. Not aware of a care plan/where things are going but have asked. Crisis calls (even from GP to psych emergency team) met with 'yes you need help' & referral back to GP or no response. Subsequent suicide attempt considered 'impulsive'. CMHT hours recently cut back and no longer cover anything out of working hours (problem as have job although currently off sick, & cover teams obviously don't know you)
21....I wasn't told of my diagnosis, despite having other issues every service is wanting me treated by the P.D. branch, I do not agree with the diagnosis of BP.D. as I do not have the required symptoms but I was never given the opportunity too challenge or even discuss the diagnosis, I only learnt of it when the crisis team were involved and the received my care plan through the post.
22....There is no psychiatrist working within my area who has an interest of specialises in P.Ds. I go private to a facility so I have to pay once a month to see a psychiatrist there who oversees my care and takes charge of the prescribing
23....My CMHT do not offer support to people with BP.D. they see you as time wasters, they've refused me support many times when I find the courage to ask for help, its so awful being turned down time and time again when you find it hard to ask in the first place
24.....No specific P.D. service, think something was started but not heard any more
25......Waiting lists to start group therapies etc. are a huge problem and lack of support groups within my area
26.......CONTINUITY OF CARE: I moved home a year ago but have not changed my GP (despite the inconvenience) because this would mean that I would also have to change my CPN, even though the CMHT that I'm under is closer to my new address. It has taken me a lot of time to build a relationship/trust/understanding with this professional and I couldn't bear to have to lose that and start all over again, simply because I've moved down the road a few miles. Before I had the diagnosis of BP.D. I was labelled a sufferer of clinical depression and was seeing a psychologist over a period of 5 years. When they retired, I was not offered any further support until I had another crisis - this left me feeling rejected and abandoned (one of the symptoms of BP.D.!). The psychiatrists at my local CMHT are constantly changing and with many of them you have a sense that they are dismissive of you anyway. The DBT that I receive is exceptional and I am very lucky to be able to take part as my inclusion was purely down to geography. However, I have anxiety about it as it is a pilot project, so funding could easily be withdrawn and there is no other DBT available in the county.
27.....I have been discharged from the CMT, I only see my Psychiatrist every 3 months and she does not know much about support someone with P.D. and I can only see her every 3 months. My GP is not the place to gain support either.
28......Lack of expertise with regard to specialist knowledge of childhood trauma. Too much reliance on medication. Being passed from one person to another (as often not sure what to do with me). Easier access to services needed, as often no out of hours support. No access here to D.B.T either.
29......Not been offered therapy was referred by Psychiatrist but was turn down for being TOO well.
30......Dissociative Identity Disorder (DID) not widely accepted. Refused talking therapy twice after therapist died. Hospital admissions within own Trust problematic and traumatic. Lack of care and empathy. Crisis service will not respond to me
31......We have no Psychologist available, I have been waiting for DBT since February and I have been informed there is no chance of it coming any time within the next few months. My Psychologist appointments are infrequent every 6 weeks and it is very hard to speak to anyone if you need help with medication problems. Also I must add the staff at (a NHS Location I go to ) are very rude when you ask for their assistance. I have been yelled at, spoken down to and ignored whilst seeking help with my treatment and I have often been left for extended periods of time on medication that I have actually been allergic too and have been having quite severe allergic reactions to. Also local GP practice misdiagnosed me for years without actually referring me to see the mental health team and they seem to have no idea what BP.D. actually is.
32.......I had DBT which didn't really work for me, although I was told MBT would be more suitable nothing ever happened. It seems as if P.D. patients get forgotten about.
33........I just don't know what is available to me or how to ask.
34........NOT MILITARY ORIENTATED
35.........Medicalisation of trauma issues
36.........Sometimes have to wait for help and someone to talk to - this cannot be helped
37........Not enough trained staff for regular sessions. or staff have other commitments.
38........Therapy being time-limited. Not time to build up a therapeutic relationship. Relationship and therapeutic alliance is key to successful treatment
39........EX Forces
40........No one apart from specialist DBT therapists understand, are trained in or are at all empathetic in my condition, most workers would rather pass the buck, this has resulted in my being abused in many ways by many services
41........Being made to feel like a hopeless case, being told that my need for stable care workers rather than unfamiliar ad hoc care is unreasonable. not being seen as a person but rather as an attention seeking manipulative P.D. who does not have a valid mental illness and is unworthy of care and support.
42.........Disability discrimination from services
43.........The staff do not care & are blatantly anti P.D.. They are abusive & do not understand my issues. Especially at (two NHS locations given)
44..........All treatment offered was short time and only for superficial aspects (the depression / anxiety I presented with) rather than treating the underlying causes.
45..........I feel that I have not been listened to
46........(The survey omits this answer due to uncertainty of its meaning)
47.........Appointments too few and far between
48..........No diagnosis. Had to diagnose myself by searching "google" extensively when I could stay on task and then have diagnosis confirmed by an independent professional. P.T.S.D. as a result of poor and inadequate healthcare unable to access NHS services for any form of healthcare. Verbally, physically and sexually abusive practices by healthcare "professionals" and no accountability No dignity, respect or empathy - Blame and shame No training in chronic pain management or understanding of MUS Incompetent GP's - poor professional boundaries, blame and transference. "Psycho" Psychologist/ PMT/ stressed/ unsure but definitely not my problem Breaches of confidentiality Patriarchal attitude toward patients No understanding of trauma A desolate wasteland of poor resources, poor skills, inadequate training, stress, incompetence and hidden abusive practices without systems of accountability CPA written and given to you to sign under duress - Professional meetings without patient consultation - No choice - treatment enforced through coercive, abusive and manipulative practices No social support, no benefits - debt Pseudo university - where have all the professionals gone? Clinical trials on vulnerable patients without informed consent. Pursuing legal action
49........Professionals (or so called) have varied opinions, therefore no consistency, my care plan is rubbish and was done without my full input, in fact my CPN is not very good at all, I can not remember when last had a review, so (am on sec 117) have insisted on one
50........Too focused on medication and taking control away from me
51........Home treatment team totally inadequate, a and e support is poor, not given access to a psychiatric doctor when in a and e have to travel out of area for wider treatment available
52.......I was in the mental health services for years (on and off) I was never offered any type of therapy until 2005 when complex needs started in (a location given) I feel I was 'dumped' there because they had no where else available.
53........Many doctors treat you like there is no hope, there's nothing they can do for you.
54.........Recovery seems to be a problem. after finishing treatment, we are not given the right support to continue recovery that hopefully will enable us to progress back into society and work.
55........Time Limited Therapy and I don't think there is any DBT therapy available, .
56........My notes have been lost on numerous occasions, and there has been a catalogue of errors in my treatment resulting in almost 2 years elapsing since the police (helped save my life ) until I got treatment.
57.......(Two crisis centre locations mentioned ) I had to go to a place for suicidal people but once you've been there you cannot go there again. However my GP is very supportive, my Psychiatrist and consultant psychotherapists are supportive even though we might not always see eye to eye...or put it this way, when I'm in a bad state I perceive everyone is angry with me.
58.......The tablets are a sort of quick fix that the NHS give to you as there are huge waiting lists to get to see a counsellor or whoever you need to help you.
59........DBT & EMDR are not available on the NHS locally and I have had to request specialist funding to access therapy privately.
60........MONEY!
61.........The only option for intensive treatment has been closed down (Henderson Hospital).
62........They don't believe me and are reluctant to diagnose or prescribe very often
63........Unhelpful G.P's and rotation of psychiatrists
64........Don't understand
65.......When presenting with bipolar symptoms I have often been treated as "attention seeking". nobody listens.
66........DBT not available in the areas I have lived in (two locations mentioned ).
67.......The Crisis Assessment & Home Treatment Team refuse referrals from people with personality disorders meaning there is little, if any, out of hours care/support.
68.......I am attending group psychotherapy based solely on people with BP.D..
69.......Not the right treatment for me and having to go all over place to find a service it there are any
70.......The trauma was caused by an assault by a doctor on NHS premises. I have difficulty receiving therapy in a similar environment. Nothing else has been offered.
71.......I waited approx. 18 months to see someone when at (a location given) and ended up seeing someone privately, which put me into substantial amount of debts.
72.......I have encountered many negative experiences. Personally, I found once I was diagnosed with BP.D., I was then labelled as a manipulative, lying, attention seeker and nothing I said was then taken seriously. I was offered a place in a Therapeutic Community but unfortunately that is not suitable as I am currently a carer for my elderly relative. I also don't agree a Democratic Therapeutic Community would be helpful for me. I was told I was "too ill" for individual therapy and also that I would only become too attached to the therapist. So I sought out private therapy and have been going weekly for 18 months. Since then we have had to seek further help due to my dissociative problems and I have now been told I probably have Dissociative Identity Disorder by private specialists. However yet again my CMHT do not take my dissociation seriously so I feel unable to tell them about my alter personalities, as I know fully well they will either put me back in hospital and dose me up on more medication or worst still, they will tell me I'm making it up for attention. I feel I have been re-traumatised by the NHS system. As a child I was not believed when I tried to tell people about the abuse I was suffering. As a teenager and an adult the disbelief has continued and caused my mental health problems to worsen. Finally I feel I must add that my local 'Crisis Team' is a joke. I have been told "Why are you phoning us? we can't stop you self harming, just make sure you go to A&E if you do something serious" and after asking for a female worker "Why? what's wrong with me?". I have friends who have also had similar problems with the crisis team.
73......Access to the same psychiatrist was never possible I met a different one on almost every visit
74......Too many to mention
75.......There is no longer access to therapy for people with the diagnosis of P.D. since the DBT programme stopped because of lack of funding. I am lucky in that I still have my therapist.
76........CMHT not very helpful at all. Organised direct payments, but no ongoing practical support and unwilling to allow access to consultant psychiatrist. Care co-ordinator seems uninterested and unwilling to help. (perhaps through overwork...or an emphasis on psychosis in the service)
77.......Once been in system 5+ years services basically withdraw
78......Insensitive inpatient psychiatrist who just threw in the diagnosis in a meeting as though I knew all about it.
79......Not being listened to
80.......I don't think psychotherapy is readily available, they use medication too freely
81.......Fragmentation of service mean that no-one will talk to one another and no-one will take responsibility - buck passing.
82.......There are no problems
83.......Psychological, physical and neglect abuse.
84...... (The survey omits this answer due to uncertainty of its meaning)
85.......No crisis help. Misunderstanding of condition leading to prejudice / judgemental treatment.
86......Lack of service input because BP.D. does not fit into NHS boxes.
87.......Medication
88.......I have moved one mile out of my area and am having to move to another trust for care and this is causing a lot of stress for me - I spent a long time building up a good relationship with the team and feel that if the patient is prepared to travel for treatment then they should be able to remain with the care team.
89.......Negative staff attitudes and lack of knowledge and information. People have responded to me based on their assumptions about me rather than my actual actions or have known less about my disorder and myself than I do but are still not prepared to listen to me. I have had a potentially life threatening illness ignored and considered to be psychosomatic until I was in A&E on a heart monitor and oxygen with a very physical problem.
90......No help at all... given Seroquel and left to my own devices... found a drug counsellor on my own!!! she is the only person I see....
91......Just keep getting put on "therapy" lists, waiting lists, waiting for assessment lists, have had two care co-ordinators, both have been limited in what care needs they can fill. Was in a psychotherapy unit full-time for one year, should have been two. as I found it impacted so greatly on my general health I pulled out but I thought I was taking part, since that need wasn't recognised or followed up, and I believe it has been noted that I "wont/cant" (not my words) work with a.n.other, then there is a reluctance to offer alternative. has been suggested I take part in social and or other activities but no help been offered or supported for my mood management, anger, helplessness etc.. I believe I am more stable but they wont uP.D.ate my care plan, in fact I have no care co-ordinator working with me at present despite having complex needs. I have noted that I have a care plan with a crisis need but this has not been signed off on, I have a carer and we say his carer assessment is poor and have argued that his needs are not being addressed. we have moved from one County to another now for care and basically we are no further on other than to suggest we drop in to their link centre ?!
92.......Counselling only 6 appointments and that's it out the door. too many changes in psychiatrists during treatment
93.......Not enough access to get you back in to mainline society
94.......No offer of any 1 : 1 therapy
95......No problems
96......A certain Senior Psychotherapist has taken against me.
97.......Lack of understanding and treatment/ diagnosis/ assessment options. just been for tertiary assessment which has lead to same / more diagnoses and have new team at staffs of which crisis and the psychiatrist (only seen once so far) seem to be working but requires a lot of coordinating by my family and myself
98........Ignorant NHS people have just made matters worse and they have destroyed any hope I have
99.......Cast aside for being aware of my surroundings and questioning them. I was diagnosed last May (2008) with P.T.S.D. when I had a very severe panic attack. My partner drove me to an A&E, I was left in a small room with no support & unable to hardly breathe. I had to ask a passing Nurse for help, I thought I was about to pass out. The other Nurses were talking over the way in full view of me-talking about the previous nights television & ignoring my obvious distress. Then all I was offered was a drugs, Quetiapine gave me horrid side effects & I had to stop taking it.
100.....The CBT Counselling had an 18 month waiting list.
101......They tell me I'm being treated for things when I am not being treated for them. symptoms of crisis are not taken into account when having them. Care co-ordinator goes on about self harm a lot but takes no notice of committing suicide which I would have thought of as a worse symptom.
102.......Being told originally that I was too nice to have a Personality Disorder by a Dr. and being treated for 4 years for Bipolar Disorder
103.....No one has time to support..
Questions 13 , 14, 15, 16 .
The survey measured User Knowledge about the Care Plan Approach (CPA)

What was strongly indicated here above is there is a "CPA-application-lag" of those who knew about the Care Plan Approach above (64.9)% and those who actually had one (34.9%). These percentages need only a very slight readjustment to indicate a truer figure due to those who answered each question (Qu. 13 = 134 and Qu. 14 = 129) . Some 51 Users (38.1%) did not even know what a CPA was .
The issue of looking into this deeper becomes more pointed when two other questions (Qu.. 3 and Qu.. 16 ) are brought into this frame of enquiry : In Qu.. 3 , 72.4% of the sample (97 people) self attributed Borderline Personality Disorder to themselves as part of their cross-condition description.
In Qu.. 16 below the survey asked who had crisis plans, a care co-ordinator, and a CPA. Out of a 132 answers 59.1% (78 Users) said they did not have any of these . That is deep cause for concern .
Teams working with people with borderline personality disorder should develop comprehensive
multidisciplinary care plans in collaboration with the service user (and their family or carers, where
agreed with the person). The care plan should:
– identify clearly the roles and responsibilities of all health and social care professionals involved
– identify manageable short-term treatment aims and specify steps that the person and others
might take to achieve them
– identify long-term goals, including those relating to employment and occupation, that the
person would like to achieve, which should underpin the overall long-term treatment strategy;
these goals should be realistic, and linked to the short-term treatment aims
– develop a crisis plan that identifies potential triggers that could lead to a crisis, specifies self management strategies likely to be effective and establishes how to access services (including
a list of support numbers for out-of-hours teams and crisis teams) when self-management
strategies alone are not enough
– be shared with the GP and the service user. "
Qu.. 15 below demonstrates the need for continuing supports in the P.D. spectrum of Users if they are to be enabled to become self helpful , more functional, and socially included . It also shows how disabling the Personality Disorder Spectrum of suffering is .

The NHS Trusts/Locations named
by each User. Question 7.
(the order has been randomised for respondent-confidentiality )
Surrey Borders NHS Trust - Epsom
Surrey & Borders NHS Trust, Stanwell, Staines
Dudley Mental Health Trust (Dorothy Pattison Hospital, Walsall)
MEDWAY PCT, CHATHAM, KENT
Sheffield Health and Social Care
Main House Northfield
Merseycare Liverpool.
Leeds partnerships NHS Foundation Trust
Castle Hill, Cottingham, Hull
Nuneaton, North Warwickshire MH Trust
South Essex Partnership NHS Foundation Trust
Bradford District Care Trust
St Georges
Carlisle
Bedfordshire and Luton Partnership NHS Trust
Oxford
Ayrshire and Arran health board
Laurel House, Canterbury Kent
North Essex Partnership, Chelmsford, Essex
Surrey and Borders Partnership Trust
South Staffs Staffordshire
Fieldhead Wakefield
Cassel hospital
Pennine Care - Bury, Lancashire
Worcestershire
Complex needs service. Tindal Centre OBMH/TVI
Lyme brook, Newcastle-Under-Lyme
Oxfordshire and Buckinghamshire Mental Health Trust High Wycombe
Worcestershire Mental Health Partnership Trust
Leeds
West Kent
2gether Foundation Trust Gloucester
no
Queen Margaret,Dunfermline,Fife
Manchester and Wandsworth
Maudsley
The Cresent in New Addington Croydon , Surrey .
Lancashire Care Foundation Trust
Main House - a residential Personality Disorder treatment in Northfield, Birmingham, part of Birmingham & Solihull Mental Health NHS Foundation Trust
Tyne and Wear, Newcastle
Hayards Heath, West Sussex
Princess Royal, Haywards Heath
Tolworth Hospital South West London and St Georges Trust
Royal Edinburgh Hospital, Edinburgh, NHS Lothian
Wallingford hospital, Oxfordshire...
Leicester and Cornwall and now Devon
Surrey, Dorking
Surrey border, Aldershot Hants
Buckinghamshire
St Leonardsgate Psychological Therapies Service St Leonardsgate Lancaster LancashireCare
Shropshire and Staffordshire foundation trust, SLAM foundation Trust
Nottingham mental health services
BSMHT
St Michaels Warwick
South Warwickshire PCT
East London
Birmingham and Solihull Mental Health Trust, Small Heath and Aston teams.
Leicestershire
Humber Mental Health Teaching Trust
Sandwell Health Authority - West Bromwich
Carters Lane House Shoreham West Sussex
Edinburgh, Lothians
South Yorkshire mental health trust, west Yorkshire
South London And Maudsley
Addenbrookes
South Essex mental health trust (Southend on sea)
Birmingham PCT North
Gateshead and South Tyneside NHS
Camden and Islington NHS foundation trust, London
Darlington
Bristol
South London and Maudsley MHT
Selby and York PCT (York)
Oxfordshire and Buckinghamshire Mental Health Trust
East London
West Herts NHS Foundation Trust Hemel Hempstead/Berkhamsted
Nottingham - Notts personality disorder network
West Suffolk CHP, then NHS Lothian.
Leicestershire
Oxford Ayelsbury, Lincolnshire
Conwy and Denbighshire health trust
North Yorkshire and York
New Craigs Hospital Inverness
CMHS fort william
Surrey and Borders NHS Partnership. Dorking
Royal Cornhill Hospital Aberdeen, Scotland
Haleacre Amersham Buckinghamshire
Cornwall and The Isles of Scilly
Derbyshire Mental health services Trust
Cassell Hospital London
Cardiff
Northampton
South West Yorkshire Mental Health Trust
Birmingham.
North Hampshire Partnership NHS trust Basingstoke
North East Wales NHS Trust
York
Northumberland, Tyne & Wear Mental Health NHS Trust, Newcastle upon Tyne
Lansdowne psychotherapy Clinic Glasgow
North Bham
North East Lincs, Grimsby
Crawley, West Sussex & Worthing, West Sussex
Lancashire Care Trust - Chorley
Wishaw North Lanarkshire
Wallingford hospital,Oxfordshire..
Lincolnshire Partnership NHS Foundation Trust
Monklands Hospital, Coatbridge, Glasgow-consultant Coathill Hospital, Coatbridge, Glasgow-psychotherapy .
QEPH Birmingham
Barnsley Community Mental Health Trust (North)
Dalston, Hackney, East London
Newtownards hospital McqQueens Department
Bootham Park Hospital, York (York and North Yorkshire PCT)
Bath & North East Somerset
South West London and St Georges Mental Health Trust
Cardiff NHS Trust.
Birmingham & Solihull Mental Health Trust
Bucks CMHT (Amersham/Haleacre Unit)
Maidstone Kent
Derbyshire PCT Newholme Hospital, Bakewell
Huddersfield- South West Yorkshire Mental Health Trust Hull
Finneston House Downpatrick County Down
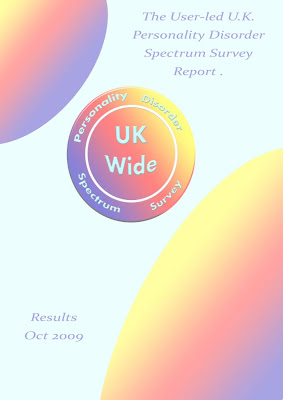
The UK Wide P.D. Spectrum Survey
Broad Findings & Trends
This first User-Led U.K. Personality Disorder Spectrum survey has shown overall (Qu. 11. ) that there are significant unmet needs for talking type therapies and for personalised choices of that too. It has shown (Qu. 16) in part of the P.D. spectrum range a lack of NHS provision for good care planning in terms of crisis and Care Plan Approaches (CPA's). It has thus strongly indicated the Care Quality Commission should pay some special attention to measuring and inspecting U.K. mental health NHS provision of comprehensive Care Plan Approaches particularly in the Borderline Personality Disorder areas where unmet CPA needs exist .
It has shown there appears to be a large NHS over-emphasis on medication even in the face of new Jan 2009 guidelines re: Borderline P.D. from NICE . It has indicated there are lack of provisions for all parts of the mental health population namely : "The P.D. Spectrum" that is simultaneously at high risk of death by suicide. Any current evolving provisions such as the Improvement to Access of Psychological Therapies (IAPT programme) must be monitored, measured, and openly reported on and certainly with a P.D. spectrum set of critical User-"spectacles" on too.
The survey has shown (Qu. 9) there is a User-need for personalised services with budgets and it has also shown there is a need for continuing care supports (Qu. 15) in this emotionally and socially disabled part of the mental health community.
It has shown crucially to Users too, that they need to see the UK picture and through organisation, monitor the UK NHS services impact upon Users. It is crucial for UK Users where they can, to take some independent ownership of the means of surveying services and to improve on that - even within the difficult context of helplessness that is often imposed upon them.
The UK mental health NHS services need to monitor and outcome measure their own provisions or lack of them, better in the P.D. spectrum and they need to make findings open. Critical well informed vision with a view to making improvements - may save lives .
There is a need for clear information both locally and nationally about P.D. spectrum patient (User) satisfaction and the 21st century has arrived with the democratisation of the Internet that can enable that . Let the UK Patient-User see what is available nationally and locally and how it is rated year on year by P.D. spectrum Users
Combat Stress and P.T.S.D.
Users with childhood related P.T.S.D. and some associated with war related combat stress individually communicated with the survey organiser and pointed out a lack of help often over years . Many stories that the survey could not contain itself were told including from Users with Dissociative Identity Disorder (D.I.D.). One such case of "Tabi Cockerton" is in the public domain . Those various stories often related to background narratives of great personal traumatic pain borne. Users spelled out what was clearly imprinted in them as revolving unassisted areas of that emotional-life-pain. Some have no therapeutic place to cry . It was reported that the NHS services often revolved Users in cycles of unresolvability , socially and personally disconnected from their admittedly often "unbearable" but unassisted selves.
Reportedly, use of drugs or inadequate solutions have been the main NHS quality recruited and human empathy was often lost . To those Users, that kind of NHS culture needs to alter towards therapeutic healing , supportive internal connection and consistent empathic external help.
Acknowledgements For Support Given :
Martin Rathfelder , Secretary of The Socialist Health Association
Malcolm Alexander , Chair of National Association For LINks Members (NALM)
Ruth Marsden , Vice Chair of NALM
Phil Lockwood Volunteer Advocate
Desmond Curley
Mandy Lawrence
Jackie Brown
Sarah Louise Brown
Tabi Cockerton
David Webb
Marjorie Lloyd
Barbara Marshall
Note : LINks = Local Involvement Networks
The User Led U.K. Wide P.D. Spectrum Survey Oct 2009
Copyright ©
(Fair-Use terms apply)
.





























.jpg)